Nursing theories
open access articles on nursing theories and models

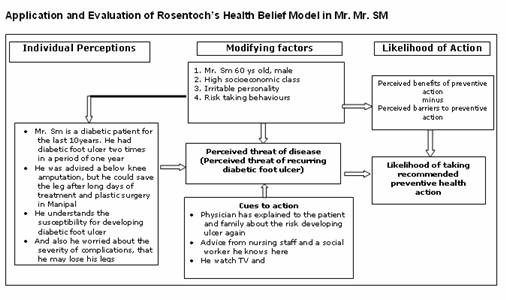
Health Belief Model (HBM)
INTRODUCTION
-
The Health Belief Model (HBM) is one of the first theories of health behavior.
-
It was developed in the 1950s by a group of U.S. Public Health Service social psychologists who wanted to explain why so few people were participating in programs to prevent and detect disease.
-
HBM is a good model for addressing problem behaviors that evoke health concerns (e.g., high-risk sexual behavior and the possibility of contracting HIV) (Croyle RT, 2005)
-
The health belief model proposes that a person's health-related behavior depends on the person's perception of four critical areas:
-
the severity of a potential illness,
-
the person's susceptibility to that illness,
-
the benefits of taking a preventive action, and
-
the barriers to taking that action.
-
-
HBM is a popular model applied in nursing, especially in issues focusing on patient compliance and preventive health care practices.
-
The model postulates that health-seeking behaviour is influenced by a person’s perception of a threat posed by a health problem and the value associated with actions aimed at reducing the threat.
-
HBM addresses the relationship between a person’s beliefs and behaviors. It provides a way to understanding and predicting how clients will behave in relation to their health and how they will comply with health care therapies.
THE MAJOR CONCEPTS AND DEFINITIONS OF THE HEALTH PROMOTION MODEL
There are six major concepts in HBM:
1. Perceived Susceptibility
2. Perceived severity
3. Perceived benefits
4. Perceived costs
5. Motivation
6. Enabling or modifying factors
-
Perceived Susceptibility: refers to a person’s perception that a health problem is personally relevant or that a diagnosis of illness is accurate.
-
Perceived severity: even when one recognizes personal susceptibility, action will not occur unless the individual perceives the severity to be high enough to have serious organic or social complications.
-
Perceived benefits: refers to the patient’s belief that a given treatment will cure the illness or help to prevent it.
-
Perceived Costs: refers to the complexity, duration, and accessibility and accessibility of the treatment.
-
Motivation: includes the desire to comply with a treatment and the belief that people should do what.
-
Modifying factors: include personality variables, patient satisfaction, and socio-demographic factors.
Criticisms of HBM
-
Is health behaviour that rational?
-
Its emphasis on the individual (HBM ignores social and economic factors)
-
·The absence of a role for emotional factors such as fear and denial.
-
Alternative factors may predict health behaviour, such as outcome expectancy (whether the person feels they will be healthier as a result of their behaviour) and self-efficacy (the person’s belief in their ability to carry out preventative behaviour) (Seydel et al. 1990; Schwarzer 1992.
REFERENCES
-
Marriner TA, Raile AM. Nursing theorists and their work. 5th ed. Sakraida T.Nola J. Pender. The Health Promotion Model. St Louis: Mosby; 2005
-
Polit DF, Beck CT. Nursing research:Principles and methods. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2007
-
Black JM, Hawks JH, Keene AM. Medical surgical nursing. 6th ed. Philadelphia: Elsevier Mosby; 2006.
-
Potter PA, Perry AG. Fundamentals of nursing. 6th ed. St.Louis: Elsevier Mosby; 2006.
-
Rosenstoch I. Historical origin of Health Belief model. Health Educ Monogr 2:334, 1974.
- Croyle RT. Theory at a Glance: Application to Health Promotion and Health Behavior (Second Edition). U.S. Department of Health and Human Services, National Institutes of Health, 2005.